ATLANTA — Even as the number of people in the hospital with COVID-19 in Georgia soared in June and, eventually, this week eclipsed the previous high from early May, the data showed no noticeable spillover into ICU rooms.
Now there's some indication that's happening.
First, an important caveat: The data the state releases for critical care bed use and availability is not specific to COVID cases - it's simply a total of how many people are using a bed, for whatever reason. If someone gets in a car wreck and needs an ICU bed, that is as much part of the data as someone with COVID.
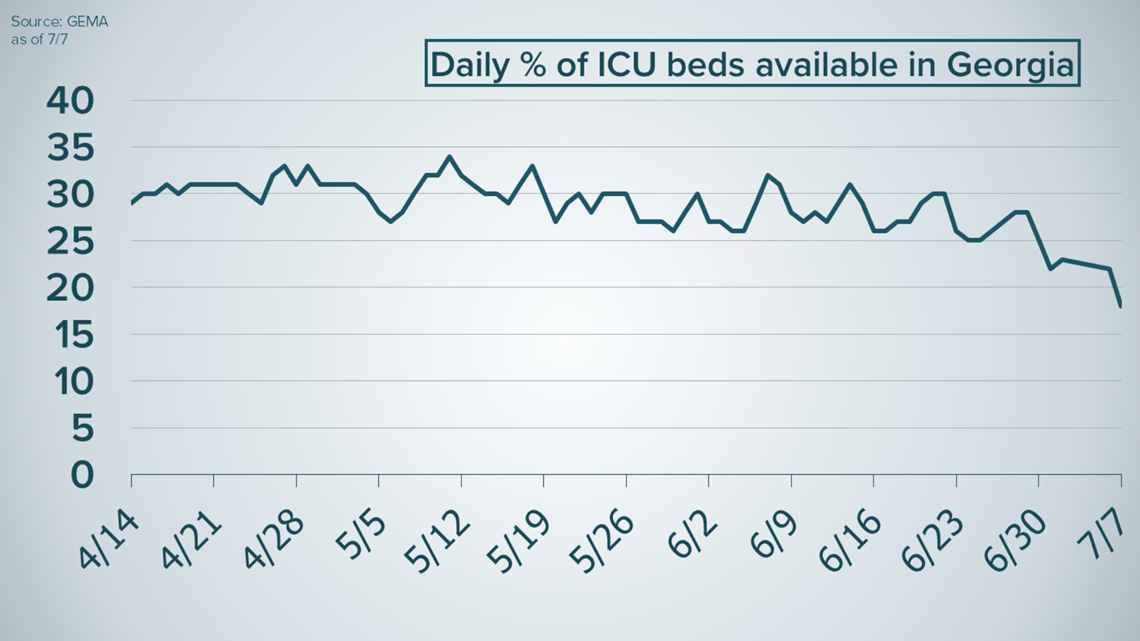
But as the chart below shows, the percent of available ICU beds in Georgia was largely stable, fluctuating mostly between 25% at the low end and under 35% at the high end throughout May and June.
On Tuesday, critical care bed availability dipped below 20% - to 18% - for the first time since Georgia began publishing that figure in mid-April.

While young people less likely to get seriously sick make up a large portion of the surging case count, even with a small percentage of serious cases a large enough case load will begin to produce substantial numbers of sicker people.
The steadily declining availability of ICU beds is a possible sign of that dynamic in play, as Georgia had a near-record day in new cases yesterday and current hospitalizations surpassed 2,000, up from 1,459 on the final day of June. The previous high was 1,500 when the state began releasing the current hospitalization number on May 1.
Ventilator use - which also does not strictly measure only COVID cases - is on the rise as well. It hit a new high of 950 yesterday, about 34% of the state's total.
Taken together, it's an indicator of the increasing - though, importantly, not yet close to debilitating - strain on hospitals in Georgia.
Dr. Jonathan S. Lewin, the CEO of Emory Healthcare, said last week the increasing number of hospitalizations presented a "high concern for overwhelming our health systems yet again."
He acknowledge that "we're not there yet, we have plenty of capacity today," but that after accounting for the lag between initially reported cases and factors like hospitalizations, "it means that in the next 3-4 weeks we're going to see an even higher surge in our healthcare system."
That doesn't mean it's a reason to panic.
Dr. Danny Branstetter, who serves as the Medical Director of Wellstar’s Infection Prevention told 11Alive's Rebecca Lindstrom last week, under normal conditions without COVID, a hospital may actually operate at a "little bit higher" capacity than we've seen with recent levels.
"Those numbers are not too concerning,” Branstetter said. "If anything, it says, 'yes, we’ve got room to take care of people.' And remember, that number does not include our surge capacity planning."
His concern was with young people contracting the coronavirus in droves.
"The one thing I want that age group particularly to know, they’re not immune to the complications of COVID infections," he said.
The steady increase in ICU bed use may be an indication that, even if young people are much less likely to get sick, if more and more of them continue to get COVID, the small percentage of them who get seriously ill will nonetheless start look like a large number.
MORE CORONAVIRUS HEADLINES

